Did you know some anaesthetic gases are hundreds or even thousands of times more harmful to the climate than CO₂? As sustainability gains momentum in healthcare, anaesthesia’s environmental impact is facing scrutiny. Anaesthetic gases typically account for around 5% of a hospital’s CO₂e emissions, but this share can rise considerably when less sustainable practices are used.
This hidden impact stems from the fact that all volatile anaesthetic gases used in operating theatres are potent greenhouse gases. They are hardly metabolised by the human body and are exhaled almost entirely into the environment. Once released, they remain in the atmosphere for years, or even more than a century in the case of nitrous oxide (N₂O). But change is underway.
The environmental cost of keeping patients asleep
Not all anaesthetic gases are created equal. Their climate impact comes down to two things: how long they stick around in the atmosphere and how powerfully they trap heat. This is called the Global Warming Potential (GWP). And the numbers are jaw-dropping. Desflurane tops the list with a GWP₁₀₀ of 2,590, meaning a single kilogram warms the planet as much as 2,590 kilograms of CO₂ over a horizon of 100 year. Isoflurane (539), nitrous oxide (273) and sevoflurane (195) score lower but are still far from harmless. Small amounts add up to a big problem.
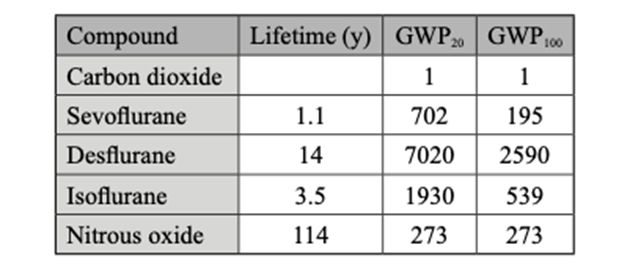
Figure 1: Atmospheric lifetimes and 20- and 100-year GWP values for anaesthetic gasses (Hendrickx et al., 2023)
The story gets worse. To keep patients asleep, anaesthetists measure doses in Minimum Alveolar Concentration (MAC). Desflurane’s high MAC means you need much more of it, piling on emissions. In fact, just one hour of desflurane-anaesthesia produces about 257 kg of CO₂e, the same as driving a petrol car from Brussels to Berlin and back. Sevoflurane, by contrast, emits only 6 kg in an hour, roughly a drive from central Paris to Charles de Gaulle Airport.
And while intravenous propofol has a far smaller climate footprint, it isn’t entirely impact-free. Small amounts enter wastewater through patient excretion and improper disposal, and laboratory studies show potential toxicity to aquatic organisms at high concentrations. Fortunately, real-world levels in hospital effluent remain far below harmful thresholds, and proper medical waste handling prevents unnecessary release into waterways.
Cutting anaesthetic emissions without compromising care
In 2023, Belgian hospitals used over 6,000 kilograms of desflurane and nearly 37,000 kilograms of sevoflurane. And yet, desflurane, despite making up just around 4% of anaesthesia cases, was responsible for almost 75% of the total climate impact. That’s a staggering imbalance. But the solution is simple: just swapping desflurane for sevoflurane could cut volatile anaesthetics-related emissions in Belgium by 73%, without affecting patient safety or clinical outcomes. While desflurane is known for slightly faster wake-up times, large-scale studies show this doesn’t significantly shorten time in post-anesthesia and so simply does not outweigh its enormous environmental cost. Other countries are already showing that such a transition is entirely feasible. NHS Scotland and England banned desflurane completely. Meanwhile, the Amsterdam University Medical Centre has gone even further by eliminating desflurane, cutting sevoflurane use by 70%, and phasing out isoflurane and N₂O altogether.
N₂O remains widely used in obstetrics and paediatrics. Its global warming impact is substantial because it persists in the atmosphere for over a century and is consumed in large volumes. Worse still, most N₂O emissions don’t even come from patients. N2O leaks straight from the central piping. In many hospitals, these systems seep gas 24/7, an invisible, silent source of pollution. So, phasing out the central piping and replace it with portable cylinders that are sealed between uses, is an easy recommendation to make.
Even when volatile agents remain in use, how they are delivered makes a big difference. This part gets a little technical, but the principle is simple: reducing waste. One of the easiest fixes is adjusting the fresh gas flow (FGF), the stream of oxygen and other gases that carries the anaesthetic into a patient’s lungs. Cutting flow from 2 litres per minute to just 0.5 litres can slash sevoflurane use by 60%. Thanks to modern anaesthesia workstations, such low flow techniques are now safe at every stage of anaesthesia, while automated gas delivery systems can fine-tune dosing for both safety and sustainability. The real spikes still come during high-flow moments (like pre-intubation) which remain hotspots for emissions.
What’s exhaled doesn’t have to be lost. Some technologies aim to reduce what is exhaled into the atmosphere. Capture systems can moderately lower emissions in controlled settings. However, their real-world contribution is currently limited: they are not widely adopted, offer only partial reduction, and recycled agent is seldom returned to clinical use. As such, capture should be seen as supplementary, and certainly not a solution that replaces more impactful actions like low-flow anaesthesia or avoiding high-GWP agents altogether.
Anaesthetic gases and PFAS
Besides the GWP-story, anaesthetic gases come with another concern: they belong to the chemical family known as PFAS, or “forever chemicals.” These substances are defined by ultra-stable carbon–fluorine bonds that nature can’t break down. Once in the air, sevoflurane, for example, degrades into trifluoroacetic acid (TFA), a persistent PFAS now turning up in rainwater, rivers, crops and even human blood. At the same time, small amounts of sevoflurane are metabolised in the body and excreted as hexafluoroisopropanol (HFIP), another long-lasting contaminant that flows straight into hospital wastewater. Neither TFA nor HFIP build up in the body in the same way as notorious PFAS like PFOA or PFOS, but their persistence means background levels keep creeping upward. More worrying still, TFA crosses the placenta and has been linked to liver damage, reduced fertility, and developmental effects suggesting today’s emissions may create tomorrow’s health risks. In other words, the same class of chemicals that made non-stick pans and firefighting foam so controversial is also hiding in the operating theatre.
Single-use anaesthesia devices
But it’s not only gases that make the operating theatre a hidden polluter. The tools and devices used every day also carry a heavy footprint, especially those designed to be thrown away after a single use. From laryngeal mask airways to intubation scopes, anaesthesia relies heavily on disposables that are convenient, sterile, and easy to source, but environmentally costly. Life-cycle assessments show a clear pattern: reusables win on almost every measure: carbon emissions, water use, waste, and even cost. Take intubation scopes: reusable models generate a fraction of the emissions compared to disposable scopes, most of which comes from producing the plastic and electronics. The same is true for laryngeal masks and anaesthetic circuits, which can be safely reused with dramatically lower impact. Hospitals that embraced reusables and reprocessed single-use devices report huge savings and far less dependence on fragile global supply chains.
Five actions hospitals can take right now
While it may seem rare in healthcare to find interventions that reduce emissions, cut costs, and protect patient safety, sustainability and smart practice often go hand in hand. Just like the case for reusable PPE, phasing out desflurane is another clear example where greener equals better. The emissions difference is striking: an anaesthetist routinely using desflurane emits more CO2e in a single year than a sevoflurane-using colleague does over an entire career, or in one month more than a total intravenous practitioner emits in a lifetime.
The message is clear: sustainability and clinical best practice go hand in hand. And the solutions are ready to implement. Based on current evidence, five immediate steps could drastically shrink the climate footprint of anaesthesia without compromising care.
- Stop using desflurane. Remove it from operating theatres altogether, hospitals in the UK and the Netherlands have already proven it can be done.
- Decommission central N₂O systems. These leaky pipelines are silent polluters. Switch to portable, sealed cylinders that only release gas when in use.
- Lower fresh gas flows. Modern workstations make low-flow anaesthesia safe. Training staff to use the lowest effective flow rate cuts consumption and emissions dramatically.
- Shift (when clinically possible) to intravenous or regional techniques. Propofol and locoregional anaesthesia carry a fraction of the climate cost compared to volatile gases.
- Switch to reusables. From laryngoscope blades to anaesthesia circuits, reusable materials are safe, proven, and slash both waste and emissions.
The operating room holds some of the clearest and most actionable opportunities for improving sustainability in healthcare. But meaningful change won’t happen by chance. At NZHI, we help hospitals turn these insights into action. Whether you're phasing out desflurane, designing low-emission clinical pathways, or building a broader sustainability strategy, NZHI can support your hospital at every stage. With our science-based tools, emission audit methods, and practical expertise, we help you align climate goals with clinical realities. From quick wins to long-term transformation, we’re here to help you move from awareness to measurable impact.
We thank Prof. Dr. Alain Kalmar for his expert review and valuable contribution to this article.
References
- Andersen et al., 2023, Assessing the potential climate impact of anaesthetic gases
- Hendrickx et al., 2023, BeSARPP (Belgian Society of Anesthesiology, Resuscitation, Perioperative medicine and Pain management) recommendations on responsible and sustainable use of inhaled anesthetics: NO time TO WASTE
- Kalmar et al., 2024, Volatile anaesthetics and PFAS forever chemicals: A critical gap in environmental impact assessments
- McGain et al., 2017, Financial and environmental costs of reusable and single-use anaesthetic equipment
- McGain et al., 2020, Environmental sustainability in anaesthesia and critical care
